Quick look:
√ Pressure injuries do not occur in people who are only confined to bed.
√ Pressure injuries occur when an individual has not been repositioned in the bed or chair (either on their own or by a caregiver).
√ They can also occur in individuals who sit in a chair or wheelchair and do not move.
√ Pressure injuries can lead to deep open areas, infection and in more severe cases, death.
Pressure injuries, also known as “bed sores” are damages to the skin or underlying tissue, usually over a boney part of the body. Pressure injuries occur when a person has not changed their position for some time. The heels and the tailbone are some of the bony areas of the skin. At first the skin may appear as a red or bruised area. Sometimes the area appears as a blister.
Not all red areas are pressure injuries. Typically, if the red area on the skin turns white right after pressure is applied (also known as “blanching”) then the red area is NOT a pressure injury
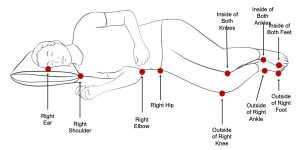
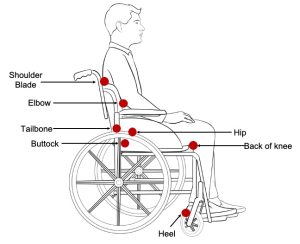
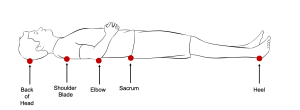
The heels and the tailbone are some of the bony areas of the skin where pressure injuries occur. Other areas where pressure injuries occur include the back of the head (occiput), ear, shoulder, shoulder blade, elbow, lower back (sacrum), hip, knees and ankles. The area where pressure injuries develop depend on what position the person is sitting in or lying in. The diagrams below show the areas that the person is at high risk of developing a pressure injury depending on what position they are lying or sitting in.
There are several ways to prevent pressure injuries from occurring which are listed below. It is much easier to prevent pressure injuries from happening than to treat them.
- Keep the pressure off: It is recommended that a person’s position in bed be changed every 1-2 hours or a person’s position in a chair be changed every 15 minutes.
- Keep the skin clean and dry: Too much moisture from urine, feces or sweat will damage the skin and cause the skin to become too soft.
- Getting enough nutrition: Nutrition is important to help the skin heal and keep it healthy.
- Use a specialty mattress: Some mattresses have special air cells that help keep the pressure off. Speak to your health care provider about getting connected with an Occupational Therapist for recommendations.
- Do not elevate the head of the bed more than 30°: If the head of the bed is elevated too high, the person will slide down in bed which can cause skin in the lower back area to break down and lead to a pressure injury.
- Use pillows and padding: For example, cover the heels with sheepskin/foam which will providing an extra layer of padding. Pillows can be used under the legs to raise the heels so they do not touch the bed.
- The pressure injury can form a channel or tunnel under the skin and into the layers of tissue.
- Skin infection. The skin or the pressure injury can become infected.
- Bone infection. The bone can become infected.
- Sepsis. Sepsis is the body’s extreme response to an infection. This can lead to tissue damage and organ failure.
- Call your primary health care practitioner (doctor or nurse practitioner) immediately.
- Find a wound care nurse.
- Take the pressure off the pressure injury.
- Check the mattress and wheelchair cushion.
- Make sure the pressure injury remains clean and dressings are changed when needed.
- Take pictures. Compare previous pictures and see if the pressure injury looks better or worse.
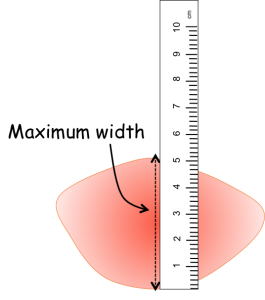
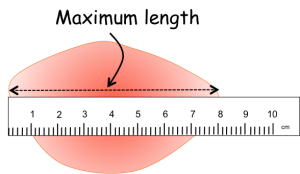
- Measure the size of the pressure injury using a ruler and document it. Measuring the size of the pressure injury over time can help you see changes in the size of the pressure injury.